What is happening with the average gut in today’s world?
The world of gut-health medicine is growing rapidly.
In the past decade, there has been an exponential growth of studies and literature supporting the importance of the health of the gut and its intact microbiome.
What is a microbiome? Think of what naturally lives inside the human body; bacteria, fungi, protozoa, and viruses, and then inside all of these lives genetic material that our bodies have grown to rely on for health and healthy guts.
But what happens when it is material our body doesn’t recognize? An unhealthy or abnormal microbiome has been implicated in both primary gastrointestinal diseases including irritable bowel, Crohn’s and ulcerative colitis, and small intestinal bowel disease (SIBO), as well as extra-gastrointestinal (conditions affecting the joints, eyes or skin) diseases. Diseases all the way from eczema to cardiovascular disease to autoimmune disease and to neurodegenerative diseases have a connection to our gut health and microbiome.
We don’t know what any individual’s perfect microbiome is yet because many factors play a role, like where and how you were born, early environmental exposures, dietary habits, medical history and medications, and even early childhood adverse events, but we are learning more and more about the roles and relationships of different species. For years we have focused on the bacterium but we see impacts from viruses, protozoa, and fungi too. An exciting time for us as we learn more!
In this issue:
- Why is Gut Health Connected to Total Health?
- What Does a Healthy Gut Look Like?
- Common Ailments That Result From an Imbalanced Gut
- Typical Treatments for Gut Ailments
- How Does Food Play a Role With a Healthy Gut?
- How Juicing Helps Create a Healthy Gut
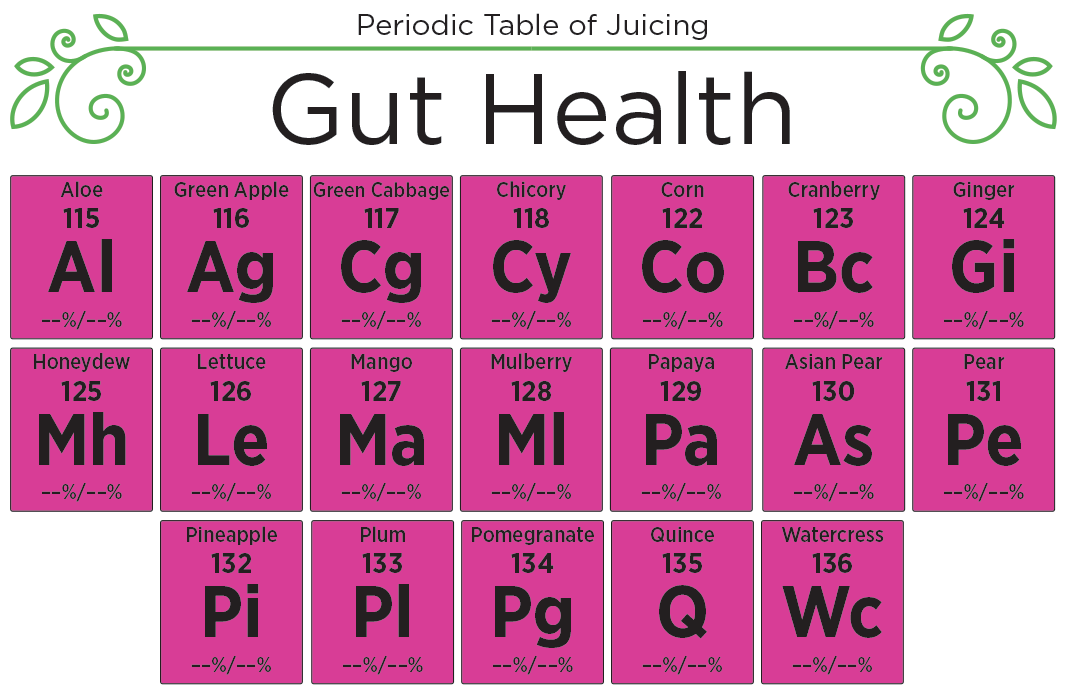
- Using the Periodic Table of Juicing for Gut Health
- Gut Health Connection
- Let’s Cleanse!
Why The Focus on Guts for ALL Health?
In recent years we have learned so much more about the mechanisms of interaction between the flora (gut flora or microbiome) of the human gut and human physiology. The species that make up our gut flora produce metabolites and mediators (tools the body uses to function properly). They have access to our whole body via the systemic and lymphatic circulation to organs such as our skin, liver, heart, muscles, and brain. Those are the two major circulatory systems we have (it is also how cancer cells metastasize). These systems give compounds, metabolites, minerals, or even pathogens access to all organs. Some organs are at less risk based on anatomical barriers (ie. the blood-brain barrier) but over time chronic inflammation breaks down those tight barriers.
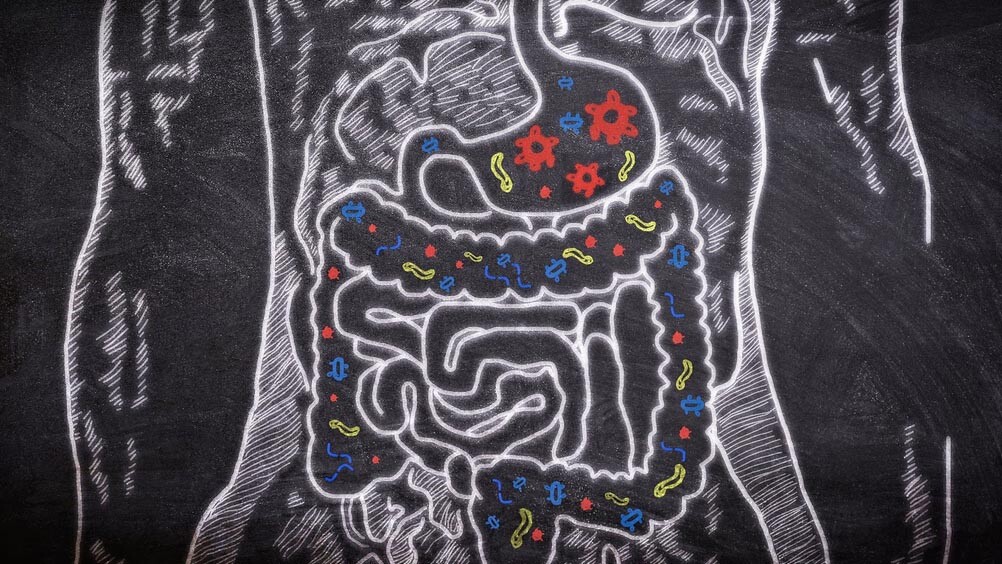
The combination of gut inflammation and an unhealthy microbiome are the root causes of an aberrant immune response that leads to damage and disease. Over time, as our gut sickens, we lose our internal ability to stop the inflammatory cascade and thus are left with a perpetual non-ending inflammatory response which can lead to immune dysfunction and mitochondrial burden (more to come about mitochondria).
What does a healthy gut look like?
A healthy gut is – to put it simply – one without inflammation. It has a variety of bacteria, microbiome, and has ‘colonization-resistance,’ meaning it naturally prevents the colonization of enteric pathogens (disease).
What happens when we lose colonization-resistance? We start the cycle of an abnormal immune response, which results in inflammation.
Understanding how inflammation is triggered in the gut is critical to gut health. Preventing inflammation will be addressed more below.

What does inflammation do to the gut? Inflammation directly changes the integrity of the mucosal lining of the gastrointestinal tract. It is inflammation that triggers both innate and adaptive immune responses, causing more inflammatory mediators to be produced. Mediators like cytokines are released as an immune response. If your body is constantly being triggered by food, environment, and stress, cytokines will constantly be released – this is chronic inflammation. This does elude to intermittent fasting but we are not going to dive into this subject today.
I also want to talk about our mitochondria, a topic that I regularly speak about at conferences.
The mitochondria is called the ‘powerhouse of the cell’ because it stores and creates energy for our cells and body from adenosine triphosphate (ATP).. If inflammation is caused by constant triggers, what happens to our energy/ATP when our body is in a constant battle in the gut? We run out of energy. Stressed cells release ATP on an as needed basis via channels in the plasma or cell membrane and vesicular export (vesicular export is the predominant mechanism for exchange of proteins and lipids between membrane-bound organelles in eukaryotic cells).. It is part of what is referred to as the ‘cell danger response’ since the cells perceive danger from all comers due to a perpetual inflammatory response. Are there foods that affect this more than others? Let’s dive into the subject of digestion.
Digestion is the conversion of complex carbohydrates via fermentation. This is a core activity of the human gut microbiome and efficient production of short-chain fatty acids (SCFA), such as butyrate, acetate, and propionate. These short-chain fatty acids are critical for the mitochondria to produce enough energy for our complex homeostatic physiology. This is what a healthy gut does and our whole body depends on our mitochondria to provide us with energy.
For those questioning the value of a plant-based diet, if you have a high-animal-protein diet, the biota (your microbiome) is forced to ferment amino acids which can produce potentially harmful compounds, such as ammonia and amines, which may result in disease. Plant-based foods do not appear to release these same compounds. Animal protein can be toxic to mitochondria both directly and indirectly via inflammation.
What are some of the common ailments that result from an imbalanced gut?
An imbalanced gut results in primary gastrointestinal diseases such as Crohn’s Disease and ulcerative colitis as well as dyspepsia and dysbiosis, irritable bowel disease, transaminitis, pancreatitis, and SIBO. But because of chronic inflammation, an imbalanced gut can cause other diseases including autoimmune disorders, cardiovascular disease, and neurodegeneration. Importantly, chronic inflammation can result in poor immune resilience to other exposures that we are all regularly exposed to over our decades of life. This includes infectious organisms, environmental toxins, contaminants, and even stress.

What are typical treatments for these ailments?
The variety of ailments from poor gut health are diverse and often require targeted treatments. There are many medications for patients, and more seemingly approved each year, but a mainstay of all treatments should include improvement and reparation of gut inflammation and altered microbiome. These treatments include nutritional intervention with improved dietary choices that are focused on the consumption of polyphenols (micronutrients packed with antioxidants), sleep hygiene guidance, use of pre and probiotics, and depending on the severity, sometimes even fecal microbiota transplantation.
I have seen many patients with poor motility, irritable bowel disease, and SIBO that have had great improvements with an improved focus on lifestyle choices.
How does food play a role in helping create a healthy gut?

Based on the explanation of digestion and our microbiome, we can safely say that food is critical for a healthy gut. Humans did not evolve to consume highly processed foods, high sugar content, or other types of food commonly found in the American diet. Complex carbohydrates and foods high in dietary fiber are key for a healthy gut. And importantly, foods with polyphenols are essential. Polyphenols are found in fruits, vegetables, nuts, flaxseeds, and even coffee. Fruits such as apples, blackberries, mulberries, black currants, and blueberries contain polyphenols. Vegetables that contain polyphenols include artichokes, spinach, chicory (endives, escarole, frisee, radicchio), and onions.
Polyphenols are potent antioxidants and have been repeatedly demonstrated to contribute to the prevention and reduced risk of chronic disease. One way in which they do this is by increasing the population of healthy bacteria such as bifidobacteria and lactobacilli. Other important compounds include oligosaccharides for appropriate fermentation of short-chain fatty acids and more energy-producing compounds. Oligosaccharides are found in blueberries, watermelons, peaches, mango, pears, and vegetables of the allicin class such as garlic, leeks, and scallions. High-fiber vegetables such as corn and those of the cruciferous classes (broccoli, cabbage, kale, etc.) further provide additional substrates (underlying substance).
Nitrates are another important compound that is produced by the microbiome and decreased by chronic inflammation. Nitrates are important for our health as they help to ensure appropriate and efficient blood supply which includes blood supply to the gut. The gastrointestinal tract has its own blood supply and when vessels are not healthy and not delivering blood to the cells of the gut, a level of ischemia (restriction) can occur which further complicates digestion, metabolism, and absorption and further damages the gut.
High concentrations of nitrates are found in green leafy vegetables such as kale, chard, arugula, cabbages, collard greens, and spinach. Beets and their leaves are known for their nitrate concentration. Other plant-based sources include watermelon, apples, bananas (which are also a great source of prebiotics), strawberries, cabbage, mushrooms, celery, and radishes.
Pineapple and ginger have enzymes that are medicinal and can relieve symptoms from inflammation including bloating, constipation, and flatulence (abdominal discomfort).
The chlorophyll that gives watercress (and other green plants) its green hue contains enzymes that are important for nutrient utilization.
Aloe vera not only balances the intestinal flora but prevents histamine release from the mast cells (part of the immune and neuroimmune systems) of the gastrointestinal tract which is an important source of inflammation from exposure to toxins, contaminants, harmful metabolites, and poorly tolerated foods.
Celery provides a detoxifying mechanism by creating an osmotic force to help the tract move waste by-products through the tract.
Fennel improves digestion and protects from worms and parasites due to the volatile oil anethole.
This is when I am grateful for my fellowship in integrative medicine, under Dr. Andrew Weil.
How can juicing specifically help create a healthy gut?
PREVENTION
When we consider juicing for healthy adults and children, we look at it as a way to consume high quantities of the compounds I mentioned above to keep our guts, mitochondria, and body strong while keeping inflammation low. We want to lead vivacious full lives with bodies that can do what they were meant to do – run, play, sleep well, love.
Drinking 16 to 32 ounces of juice a day allows us to nourish our bodies along with supporting our guts to digest a robust plant-based diet. Juicing has been found to create high quantities of nitric oxide which decreases inflammation (1) This works for preventing inflammation. When you combine juicing with a plant-based lifestyle, you are adding more fuel to your body and giving it more tools to heal and thrive.
We love seeing families juice. Prevention ideally starts at a young age so our children are strong and resilient as they face the Standard American diet.

HEALING
Healing the gut requires the same juice but a different strategy. If we are living with inflammation and most often a fatigued immune system, we want to drink more juice (32oz or more) to nourish our hungry body so it can gently restore the gut. Juicing has been found to create high quantities of nitric oxide which decreases inflammation (1).
Consuming primarily whole plant-based foods is always ideal, but if a gut is damaged, it will be difficult for the gut to efficiently digest these foods which may not only lower the bioavailability of the nutrients and compounds but may even further contribute to inflammation and gut discomfort.
A cold-pressed juice contains nutrients and compounds without the fibrous components that may be difficult for the inflamed gut to handle. It may be hard to digest it to the purest state. That is why juicing plant foods, especially the ones suggested above, and drinking them throughout the day is one of the most healing ways to build your gut back to health.
If really committed, then an estimated healing time is 3 months.

When our bodies are feeling more energized, we will continue to juice and return to a more robust diet with whole plant-based foods. Juicing again complements what we eat to create a beautiful harmony with the nutrients we eat throughout the day. We recommend 16 to 32 ounces a day. If we notice our energy levels are low or if our gut feels off, we can always go back to more juices to feed our bodies.
Juicing not only helps to heal but protects during the healing process. And then, as a bonus, drinking juice prevents recurrence of inflammation and can be protective. Juicing ensures our bodies can absorb and assimilate these compounds without the burden of digestion which can be stressful for a stressed-out gut.
Using the Periodic Table of Juicing for Gut Health
Some of my favorite ‘elements’ in the gut-health category include berries, Asian pears, pineapples, and green leafy vegetables. I regularly juice aloe vera, celery, and ginger when my gut needs some TLC. Combine them in any way that sounds delicious to you. There are no rules to juicing. Just juice and enjoy. But if you prefer recipes, here are a few that I recommend for my patients:
- Simple Green: Pure celery juice (mono-juicing!)
- Rise and Shine: Asian pear, ginger, dandelion, or other edible flowers
- Do the Dew: Honeydew, arugula, green cabbage
- Homerun: Apple, fennel, pomegranate, watercress
- Let Us Be: Lettuce, cranberry, spinach
- Walk on the Wild Side: Banana, papaya, mango (We recommend freezing the fruits and using stage one to create a smoothie bowl with these ingredients).
Video demos to come!
Gut Health Connection
I have seen many patients over the years with various symptoms that often include a history of poor gut function. Many times, there is chronic constipation which only results in waste stasis and leads to dysmotility and stagnation, and SIBO. Over time, the unhealthy microbiome creates an environment of inflammation and toxicity allowing mediators and compounds access to the circulation and creates end-organ damage, often on a cellular level years before true disease results. Oftentimes, once the disease is present, it can be harder to completely reverse the damage.
But working on healing the guts and regenerating a healthy membrane lining of the tract can help minimize symptoms and hopefully slow the progression of the disease. It is very possible that most modern-day maladies stem from poor gut health which in most cases, starts when we turn to poor foods and lifestyle choices. Gut health isn’t completely dependent on the foods we choose to eat but also on how active we are, how well we sleep, and how we manage stress also play a role.

Join Me!
I too have been in a rut and have been so busy and overwhelmed with life and its many obligations that I have not been true to my preach. This blog has reminded me how important self-care and self-nurturing are because we are the only ones that can care for our own bodies. Excuses only hurt ourselves. My resolve is renewed to return to what I know best for myself and my health.
Thank you for following me on this journey through the Periodic Table of Juicing. We welcome your comments and questions below. I do not give medical advice in these comments so please ask your local doctor for specific medical advice.
Next month, we will be discussing one of my favorite subjects (I am a neurologist after all), the brain!
1 Health benefit of vegetable/fruit juice-based diet: Role of microbiome.
Henning SM, Yang J, Shao P, Lee RP, Huang J, Ly A, Hsu M, Lu QY, Thames G, Heber D, Li Z.Sci Rep. 2017 May 19;7(1):2167.
Human Gut Microbiome: Function Matters.
Heintz-Buschart A, Wilmes P.Trends Microbiol. 2018 Jul;26(7):563-574.
The gut microbiota and host health: a new clinical frontier.
Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, Hold G, Quraishi MN, Kinross J, Smidt H, Tuohy KM, Thomas LV, Zoetendal EG, Hart A.Gut. 2016 Feb;65(2):330-9.
Diet and the Human Gut Microbiome: An International Review.
Wilson AS, Koller KR, Ramaboli MC, Nesengani LT, Ocvirk S, Chen C, Flanagan CA, Sapp FR, Merritt ZT, Bhatti F, Thomas TK, O’Keefe SJD.Dig Dis Sci. 2020 Mar;65(3):723-740
Gut Microbiome: Profound Implications for Diet and Disease.
Hills RD Jr, Pontefract BA, Mishcon HR, Black CA, Sutton SC, Theberge CR.Nutrients. 2019 Jul 16;11(7):1613.
Influence of diet on the gut microbiome and implications for human health.
Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, Abrouk M, Farahnik B, Nakamura M, Zhu TH, Bhutani T, Liao W.J Transl Med. 2017 Apr 8;15(1):73.
Food Components and Dietary Habits: Keys for a Healthy Gut Microbiota Composition.
Rinninella E, Cintoni M, Raoul P, Lopetuso LR, Scaldaferri F, Pulcini G, Miggiano GAD, Gasbarrini A, Mele MC.Nutrients. 2019 Oct 7;11(10):2393.
The effects of plant–based diets on the body and the brain: a systematic review.
Medawar E, Huhn S, Villringer A, Veronica Witte A.Transl Psychiatry. 2019 Sep 12;9(1):226.
Mediators of Gut Mucosal Immunity and Inflammation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4417598/
Mediators of Inflammation and Immune Responses in the Human Gastrointestinal Tract
https://www.hindawi.com/journals/mi/2013/865638/
On the Mechanism of ATP Hydrolysis in F1-ATPase